Overview
Female urinary system
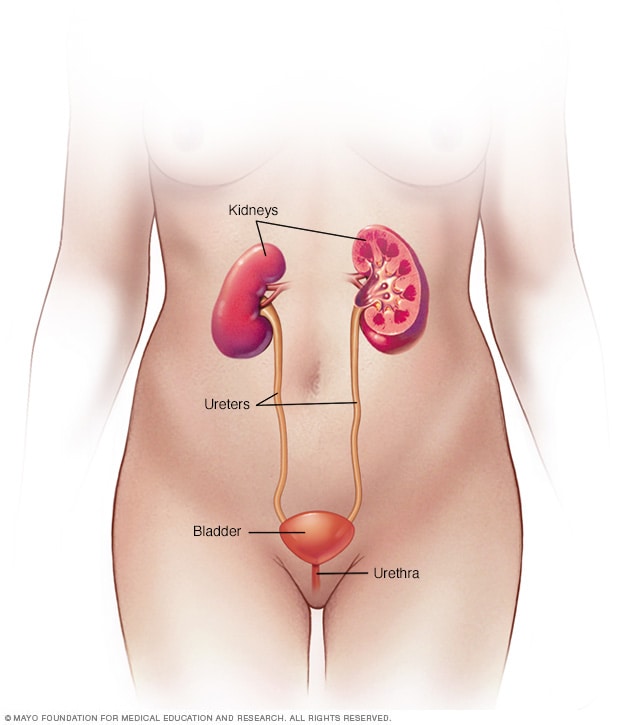
Female urinary system
Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
Male urinary system
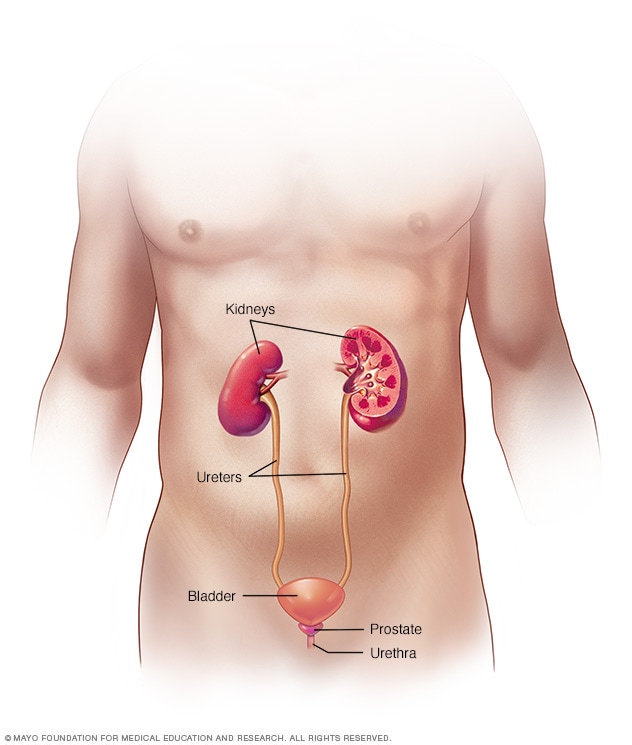
Male urinary system
Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux is the abnormal flow of urine from your bladder back up the tubes (ureters) that connect your kidneys to your bladder. Normally, urine flows from your kidneys through the ureters down to your bladder. It's not supposed to flow back up.
Vesicoureteral reflux is usually diagnosed in infants and children. The disorder increases the risk of urinary tract infections, which, if left untreated, can lead to kidney damage.
Children may outgrow primary vesicoureteral reflux. Treatment, which includes medication or surgery, aims at preventing kidney damage.
Products & Services
Types
Symptoms
Urinary tract infections commonly occur in people with vesicoureteral reflux. A urinary tract infection (UTI) doesn't always cause noticeable signs and symptoms, though most people have some.
These signs and symptoms can include:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- The need to pass small amounts of urine frequently
- Cloudy urine
- Fever
- Pain in your side (flank) or abdomen
A UTI may be difficult to diagnose in children, who may have only nonspecific signs and symptoms. Signs and symptoms in infants with a UTI may also include:
- An unexplained fever
- Lack of appetite
- Irritability
As your child gets older, untreated vesicoureteral reflux can lead to:
- Bed-wetting
- Constipation or loss of control over bowel movements
- High blood pressure
- Protein in urine
Another indication of vesicoureteral reflux, which may be detected before birth by sonogram, is swelling of the kidneys or the urine-collecting structures of one or both kidneys (hydronephrosis) in the fetus, caused by the backup of urine into the kidneys.
When to see a doctor
Contact your doctor right away if your child develops any of the signs or symptoms of a UTI, such as:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Abdominal or flank pain
Call your doctor about fever if your child:
- Is younger than 3 months old and has a rectal temperature of 100.4 F (38 C) or higher
- Is 3 months or older and has a fever of 100.4 F (38 C) or higher and seems to be ill
- Is also eating poorly or has had significant changes in mood
Causes
Your urinary system includes your kidneys, ureters, bladder and urethra. All play a role in removing waste products from your body via urine.
Tubes called ureters carry urine from your kidneys down to your bladder, where it is stored until it exits the body through another tube (the urethra) during urination.
Vesicoureteral reflux can develop in two types, primary and secondary:
-
Primary vesicoureteral reflux. Children with primary vesicoureteral reflux are born with a defect in the valve that normally prevents urine from flowing backward from the bladder into the ureters. Primary vesicoureteral reflux is the more common type.
As your child grows, the ureters lengthen and straighten, which may improve valve function and eventually correct the reflux. This type of vesicoureteral reflux tends to run in families, which indicates that it may be genetic, but the exact cause of the defect is unknown.
- Secondary vesicoureteral reflux. The cause of this form of reflux is most often from failure of the bladder to empty properly, either due to a blockage or failure of the bladder muscle or damage to the nerves that control normal bladder emptying.
Risk factors
Risk factors for vesicoureteral reflux include:
- Bladder and bowel dysfunction (BBD). Children with BBD hold their urine and stool and experience recurrent urinary tract infections, which can contribute to vesicoureteral reflux.
- Race. White children appear to have a higher risk of vesicoureteral reflux.
- Sex. Generally, girls have a much higher risk of having this condition than boys do. The exception is for vesicoureteral reflux that's present at birth, which is more common in boys.
- Age. Infants and children up to age 2 are more likely to have vesicoureteral reflux than older children are.
- Family history. Primary vesicoureteral reflux tends to run in families. Children whose parents had the condition are at higher risk of developing it. Siblings of children who have the condition also are at higher risk, so your doctor may recommend screening for siblings of a child with primary vesicoureteral reflux.
Complications
Kidney damage is the primary concern with vesicoureteral reflux. The more severe the reflux, the more serious the complications are likely to be.
Complications may include:
- Kidney (renal) scarring. Untreated UTIs can lead to scarring, which is permanent damage to kidney tissue. Extensive scarring may lead to high blood pressure and kidney failure.
- High blood pressure. Because the kidneys remove waste from the bloodstream, damage to your kidneys and the resultant buildup of wastes can raise your blood pressure.
- Kidney failure. Scarring can cause a loss of function in the filtering part of the kidney. This may lead to kidney failure, which can occur quickly (acute kidney failure) or may develop over time (chronic kidney disease).
Feb. 11, 2022